A polyp is an abnormal growth of tissue that attaches itself to the inner lining of an organ. It appears flat and roundish and is mostly less than half an inch in size. Polyps may grow in the colon (large intestine), ear, nose or uterus.
What is a polypectomy procedure?
The procedure to remove a polyp is known as a polypectomy.
A polyp in the colon is usually detected through a colonoscopy in which a thin, elongated tube with a camera (colonoscope) is inserted into the rectum. If found, the polyp is then removed through a polypectomy in the same sitting.
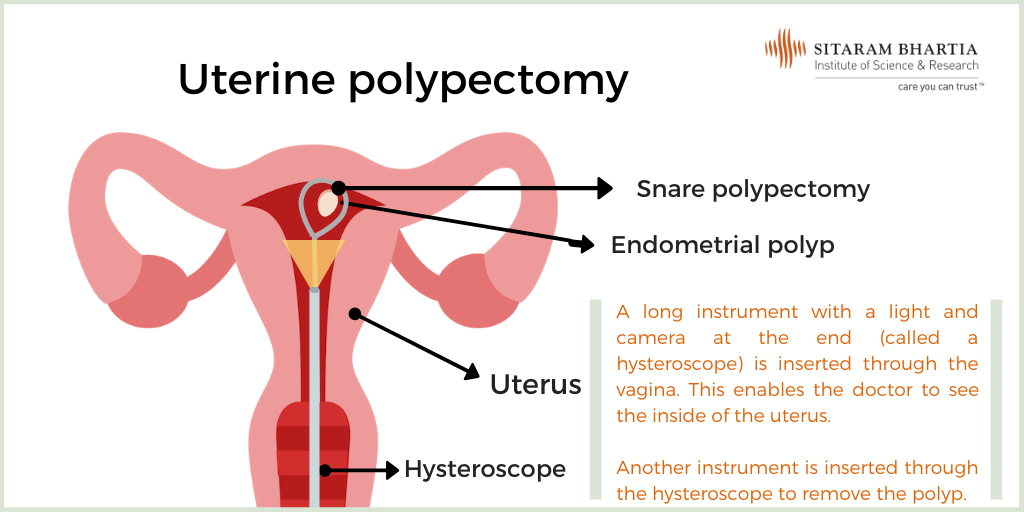
Polyps in the uterus, called uterine or endometrial polyp, are taken out through a hysteroscopic polypectomy.
How do I know I have a polyp?
Most often polyps do not cause symptoms and go undetected.
Polyps in the colon at times may cause blood in stool, pain or a change in your bowel patterns.
“If you experience symptoms like unusual, heavy or painful bleeding, postmenopausal bleeding, pelvic pain or difficulty getting pregnant, we may suggest a hysteroscopy to diagnose the cause of your symptoms, “ says Dr. Priti Arora Dhamija, Senior Gynecologist & Fertility Expert at Sitaram Bhartia Hospital in South Delhi.
If an ultrasound or other imaging test reveals the presence of a polyp, your doctor may advise removing it through a hysteroscopy and polypectomy.
What is a hysteroscopy and polypectomy?
In a hysteroscopy, a hysteroscope which is a long, thin tube with a camera and light at one end is inserted into the vagina, cervix and then the uterus. This tube helps the gynecologist see the inside of the uterus.
Instruments are inserted through the hysteroscope into the uterus to remove the polyp.
Is a polypectomy painful?
It may feel slightly uncomfortable to have a hysteroscope or colonoscope inserted into your body but the process of removing the polyp itself or the polypectomy is not painful.
How should I prepare for the procedure?
Preparing for Polypectomy of the Colon
Your bowel consists of the colon and rectum. The rectum contains the waste matter before it is excreted out of the body. Since the colonoscope is inserted into the rectum, it needs to be cleared of any matter before the procedure.
“You will be asked to clear out your bowel a day or two before the procedure. This can be done by consuming a liquid based diet and by taking laxatives if necessary.”
You will be advised not to eat or drink about 6 hours prior to the procedure.
What to expect at the hospital
In a pre-anesthetist check up a few days prior to the procedure, the anesthetist will take a history to understand whether you have previously had any reactions to any anesthetic. You will be asked to change into a hospital gown and lie down on your side on the examination table. A gastroenterologist will perform the procedure.
The anesthetic that is administered may make you feel drowsy.
Duration of the colonoscopy and polypectomy
The polypectomy takes less than half an hour but the entire procedure may take about an hour, depending on the size of the polyp.
Preparing for a uterine polypectomy
What to expect
A polypectomy for an endometrial polyp is performed by a gynecologist in the operation theatre. “In much the same way as a polypectomy in the colon, you will be asked to fast for 6 hours before the procedure.”
You will be given general anesthesia.
The process can take between 15-20 minutes.
Uterine polypectomy recovery
“You can go back home the same day after your polypectomy.” It is not uncommon to observe light bleeding or pain for the next few days. You can rest for a day or two or if you prefer, you can resume your daily routine.
“If you experience nausea or shivering, you should contact your doctor,” cautions the doctor.
Do all polyps need to be removed?
If the polyp is not causing any symptoms, your doctor may suggest waiting a while before recommending any course of action.
If, however, the polyps are found to be the reason behind abnormal bleeding or pain, it is best to remove them.
The benefit of getting a polypectomy is that the growth can be examined or sent for a ‘biopsy’ to determine whether it is benign, pre-cancerous or malignant.
It is performed as a day care procedure and doesn’t require making any cuts or incisions. You may be asked to stay in the hospital for a few hours after which you can return home.
There are a few risks such as bleeding or infection.
Types of polypectomy
The type of a polypectomy advised depends on the size of the polyp.
Snare polypectomy: This is performed for polyps larger than 1 cm in diameter. In this procedure, a loop is swung over the polyp and the mass is removed from the base using heat.
Biopsy forcep: For polyps smaller than 5 mm in size, a biopsy forcep may be used. Forceps are inserted through the telescope and placed over the polyp so that it is ‘bitten off’ and removed.
Sunaina’s experience of a uterine polypectomy
When Sunaina Dewan, 52, experienced heavy bleeding after menopause, she was recommended a hysteroscopy.
“The doctor explained that if they found polyps or abnormal growths in the uterus, it may be better to remove them there and then,” says Sunaina.
“I was sceptical and had many apprehensions but the doctor cleared each of them.”
“I understood that polyps could cause heavy bleeding and leaving them in may cause the bleeding to continue. They may even increase in size or turn cancerous.”
“We asked Sunaina to get a few blood investigations to evaluate her fitness for the procedure,” advises Dr. Priti.
“Once she was deemed fit, we scheduled a date.”
The procedure went well. Sunaina says, “ Since I was under anesthesia, I didn’t really feel anything. My gynecologist informed me that a polyp was not only detected but also removed. “
“While hearing that relaxed me, I realized that my real test would be in the week I waited for the biopsy results.”
“It was nerve-wracking. So you can imagine my relief when I found out the polyp was benign.”
“In retrospect, I’m glad I didn’t take a chance and didn’t ignore the bleeding. If I had waited any longer, the polyp may have grown and caused more problems,” completes Sunaina.
This blog post has been written with editorial inputs from Dr. Priti Arora Dhamija, Senior Obstetrician-Gynecologist with a keen interest in fertility and pelvic endoscopy.
 Medically Reviewed by Dr. Priti Arora Dhamija
Medically Reviewed by Dr. Priti Arora Dhamija
MBBS, Maulana Azad Medical College, Delhi (1999); M.D, Lady Hardinge Medical College (2004); DNB Obstetrics & Gynecology (2004); Diploma in Pelvic Endoscopy, Kiel, Germany (2014)
Experience: 17 years
More Resources:
- Going for a Hysteroscopy? Here’s All You Need to Know About It
- Endometrial Polyps: Do You Require Treatment?
- Fibroid Treatment Without Surgery: Is That the Right Option?